Insurers cut back GLP-1 coverage as demand soars: Found study

As demand surges for GLP-1 therapies, insurers are pulling back on coverage, according to new data from obesity care provider Found. | Sarah Jones Simmer, CEO of Found, said that the trends are likely the result of irresponsible prescribing for recreational reasons causing the pendulum to swing "all the way in the other direction," and it's leading to patients who have genuine medical need struggling to access these therapies.

Focus: US diabetes patients face delays as insurers tighten Ozempic coverage

Ozempic coverage is reduced under Ontario Drug Benefit Plan

IPN 2023 January by IPN Communications LTD - Issuu

Consensus Recommendations on GLP-1 RA Use in the Management of

The Doctor Prescribed an Obesity Drug. Her Insurer Called It 'Vanity.' - The New York Times
/sites/default/files/styles/embed_xxl/p
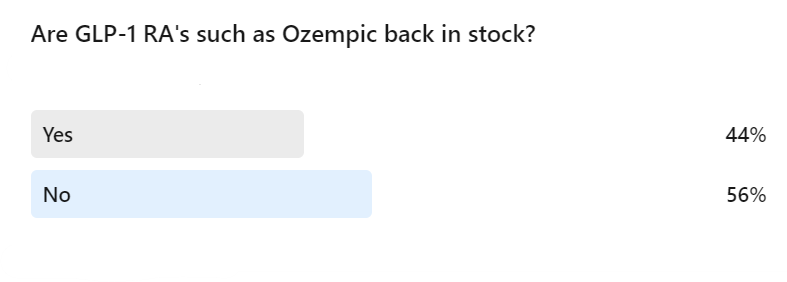
GLP-1 Receptor Agonist Shortage: Challenges and Solutions in Type

www.usnews.com/dims4/USNEWS/2c0677c/2147483647/thu

The Internet, Search Frictions and Aggregate Unemployment - Edward

Diabetes patients facing insurance hurdles getting GLP-1s: report (NVO)
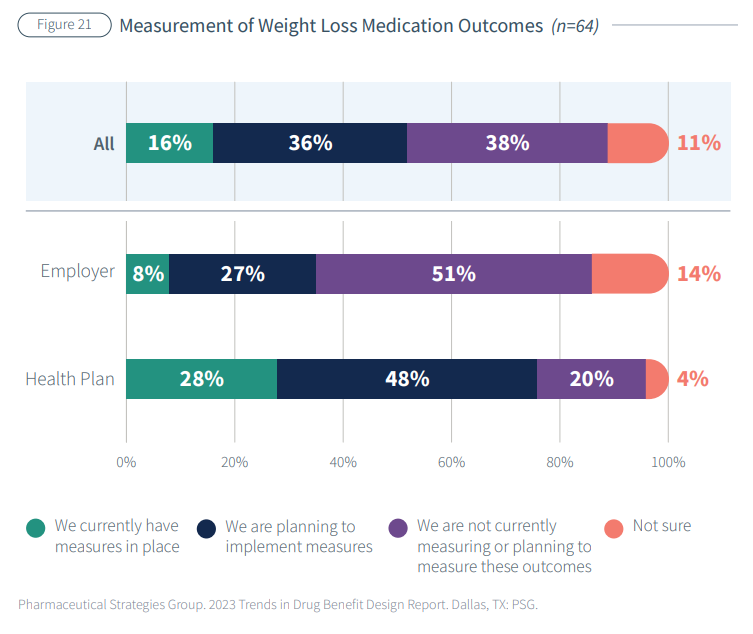
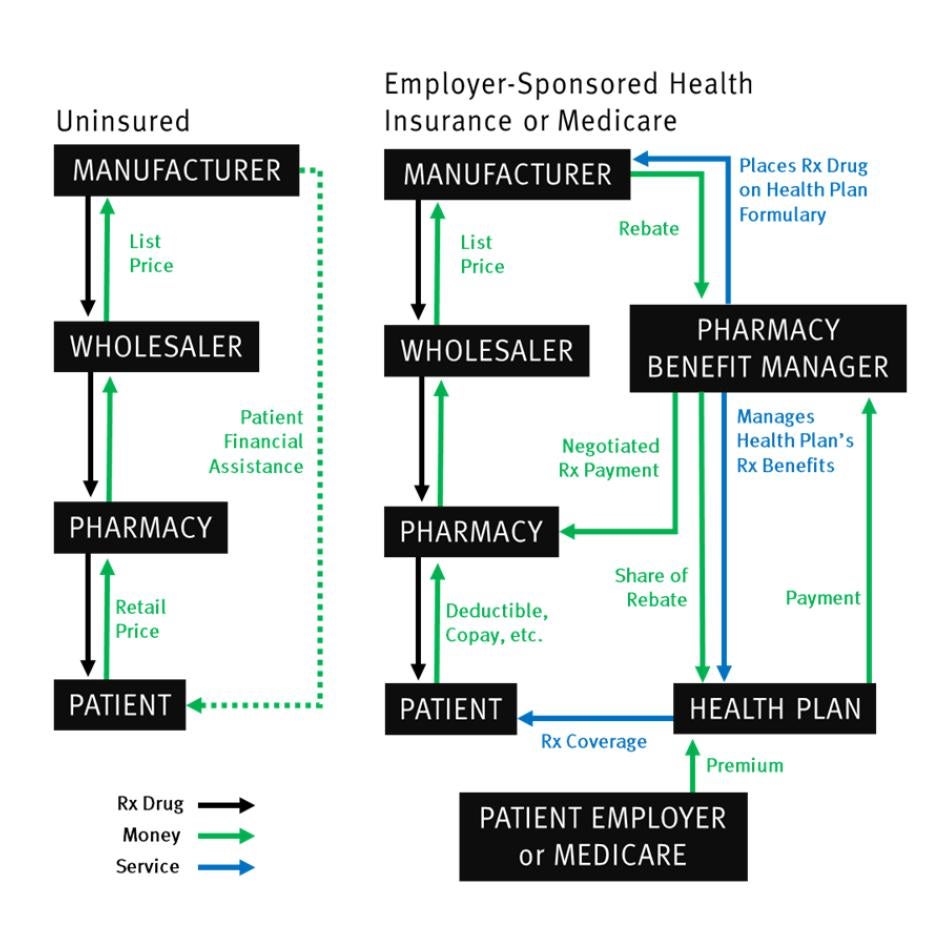
Why payers are hesitant to cover GLP-1 drugs for weight loss

Tsunami of exclusion': Patients face aftermath of GLP-1 cuts
:max_bytes(150000):strip_icc()/Samsung-Note-Edge-Tut-01-56a761923df78cf7729568c7.jpg)