GPs' identification of patients with mental distress: a coupled questionnaire and cohort study from norwegian urban general practice, BMC Primary Care
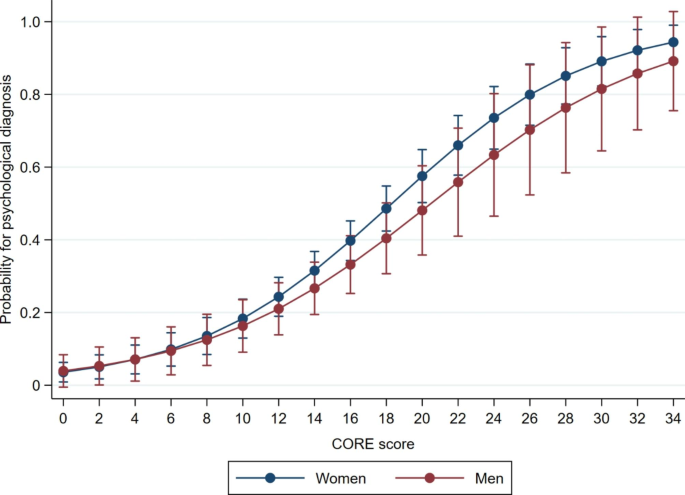
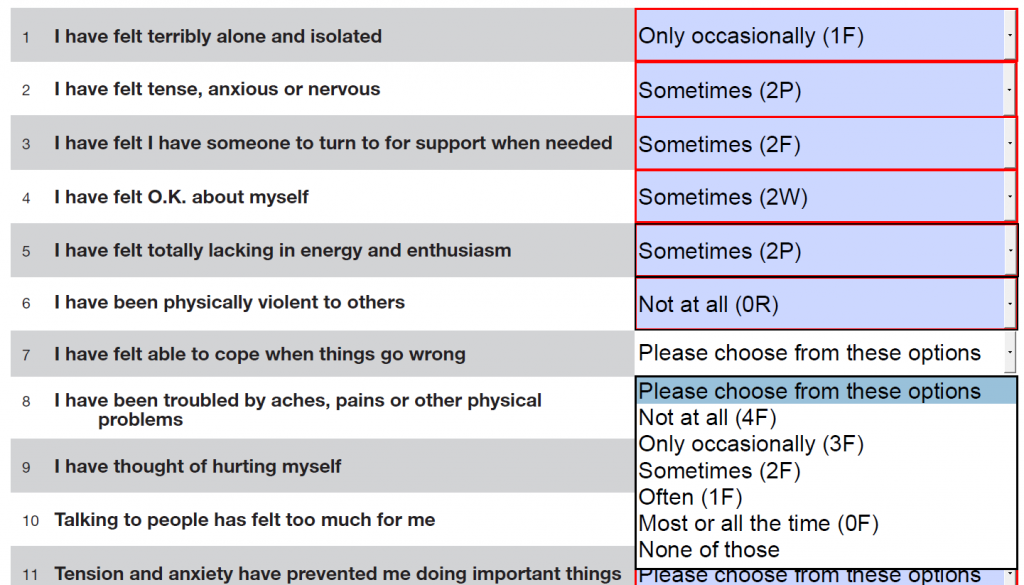
Background Mental health problems are one of the leading causes of disease burden worldwide, and are mainly diagnosed and treated in general practice. It is unclear however, how general practitioners (GPs) identify mental health problems in their patients. The aim of this study was to explore how patients’ self-reported levels of mental distress correspond with psychological diagnoses made by their GPs, and associations with sex, age, number of consultations, and somatic symptom diagnoses. Methods A questionnaire study coupled with retrospective and prospective cohort data from 553 patients aged 16–65 years in six GP offices in Oslo, Norway during 21 months in 2014–2016. Results We found that 73.3% of patients with self-reported high levels of mental distress versus only 13.3% of the patients with low levels of mental distress had received a psychological diagnosis (p < 0.01). We found an increase in number of consultations for the group with high levels of mental distress regardless of having received a psychological diagnosis (p < 0.01). There was also an increase in number of somatic symptoms (p = 0.04) and higher number of females (0.04) in this group. 35% of patients had received one or more psychological diagnosis by their GP. Mean CORE-10 score, being female and a high number of consultations was associated with having received a psychological diagnosis. In the adjusted analyses high CORE-10 score and a high number of consultations still predicted a psychological diagnosis. Conclusions We found a clear association between self-reported mental distress and having received a psychological diagnosis amongst the participants, and the probability for being identified increased with increasing levels of mental distress, and increasing number of visits to their doctor. This suggests that GPs can identify patients with high levels of mental distress in general practice in an adequate way, even though this can sometimes be a complex issue. Trial registration Trial registration The main study was retrospectively registered in ClinicalTrials.gov on August 10 2019 with identification number NCT03624829.

Facilitators and barriers of implementation of routine postnatal care guidelines for women: A systematic scoping review using critical interpretive synthesis — JOGH

Torleif Ruud - Institute of Clinical Medicine
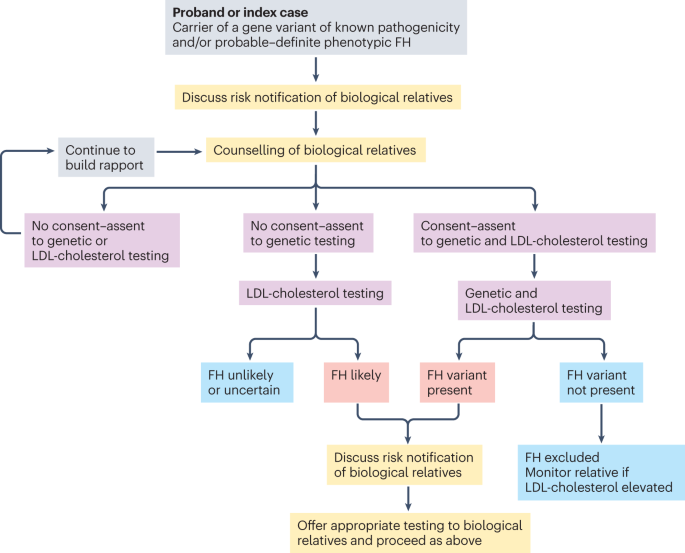
International Atherosclerosis Society guidance for implementing best practice in the care of familial hypercholesterolaemia

Patterns of Mental Health Care in Remote Areas: Kimberley (Australia), Nunavik (Canada), and Lapland (Finland): Modèles de soins de santé mentale dans les régions éloignées: Kimberley (Australie), Nunavik (Canada) et Laponie (Finlande)

DJPH - Homelessness, Poverty, and Public Health by Delaware Academy of Medicine and the Delaware Public Health Association - Issuu
Pharmaceuticals, Free Full-Text
Frontiers A Public Mental Health Study Among Iraqi Refugees in Sweden: Social Determinants, Resilience, Gender, and Cultural Context

Telehealth - Wikipedia

PDF of Finalized FAQs with Background - Alliance for Academic

Impact of relational continuity of primary care in aged care: a systematic review, BMC Geriatrics

2021 International Cancer Education Conference Program and Abstracts. - Abstract - Europe PMC